
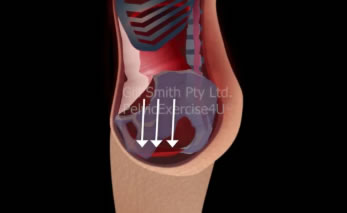
Pelvic Organ Prolapse is a condition that can happen to women. It occurs when organs in the pelvis, like the bladder, uterus, or rectum, move from their normal position and bulge into the vagina. It can cause discomfort, pressure, or even pain. Researchers wanted to find out if there was a connection between the position of the pelvis and rectal prolapse.
The study involved two groups of patients.
One group had rectal prolapse, and the other group didn't have any bowel problems. The researchers measured the angle of the pelvis using a special tool called a pelvic goniometer. They put the patients into three categories based on the angle of their pelvis: posterior pelvic tilt, neutral pelvis, or anterior pelvic tilt.
The results showed that patients with rectal prolapse were more likely to have a posterior tilt in their pelvis than those without prolapse. This means that their pelvis was tilted backward. The researchers also found that having a posterior tilt in the pelvis was a significant risk factor for rectal prolapse.
Knowing about the connection between the position of the pelvis and rectal prolapse can help Pelvic Health practitioners better prevent and manage the condition. If you are experiencing symptoms of pelvic organ prolapse, such as a feeling of pressure or bulging sensation in the vagina, it's important to talk to your doctor to make sure that feeling is a pelvic organ prolapse and then seek help from a Pelvic Health Physio.
It's important to take care of your pelvic health and talk to your doctor if you have any concerns.
Remember that there are ways to manage pelvic organ prolapse, and understanding the risk factors can help with prevention and treatment.
Reference:
Cantiani, C., Sgamma, D., Grossi, E. et al. Posterior pelvic tilt is a risk factor for rectal prolapse: a propensity score matching analysis. Tech Coloproctol 24, 463–469 (2020). https://doi.org/10.1007/s10151-020-02179-9
https://rdcu.be/c8DJd

Marilyn continued to experience bothersome period-type pain, prompting her to seek medical advice from her regular GP. Blood tests and ultrasound scans showed no abnormalities, but Marilyn mentioned that the GP who did her PAP smear had previously diagnosed POP. Her regular GP then referred her to a gynaecologist for further evaluation. The gynaecologist performed an examination, which revealed no significant concerns about the stage of Marilyn's POP. However, no assessment was performed to check the quality of her pelvic floor muscle contraction or if the pelvic floor muscles were intact. Marilyn was then given two ring pessaries to trial, but both were pushed down, and felt uncomfortable after 24 hours. While Marilyn was able to pass stools successfully with the pessary in situ, the gynaecologist requested that she stop using it. Marilyn persisted with her daily PFMT routine and was eventually referred to a urologist specializing in POP surgery after requesting a referral from her GP. The urologist diagnosed Marilyn with moderate POP but did not mention the stages of POP to her. The urologist then recommended that Marilyn be reviewed by a pelvic health physiotherapist specializing in teaching PFMT and return for a follow-up assessment in six months if she still experienced bothersome symptoms. The referral to a pelvic health physiotherapist took two years from the initial diagnosis of POP. Upon examination by the pelvic health physiotherapist, Marilyn had moderate to strong pelvic floor muscle strength, however, Marilyn performed a significantly bearing down pattern at the end of her pelvic floor muscle contraction and increased intra-abdominal pressure (IAP) on her pelvic floor. The treatment focused on restoring the correct action of Marilyn's pelvic floor muscles without the bearing down component to enhance pelvic floor muscle strength. The clinical reasoning regards why the pessary was not successful, could have been due to Marilyn trying too hard and adding a significant bearing down pattern, pushing the pessaries downward, There may have also been issues with Marilyn practicing the incorrect motor control pattern of her pelvic floor muscles for 30 years, contributing to the development of POP bother.